On Monday, May 1, 2017, Dr. David Jacobs, Chief Scientist for NCHH and a representative of the National Safe and Healthy Housing Coalition, testified before the U.S. Environmental Protection Agency about the potential dangers of weakening or terminating the existing lead renovation, repair, and painting (RRP) and abatement regulations. Three days later, Dr. Jacobs submitted this formal written testimony, reprinted below. This is one of a series of actions by NCHH and its allies to support continued (and increased) funding for the EPA's lead poisoning prevention program. You can also read Dr. Jacobs' blog, "Threats or Promises," or the letters to EPA Administrator Pruitt and to Congress, for which we are collecting signatures through May 8. Sign here.May 4, 2017
Sarah Rees, Director
Office of Regulatory Policy and Management
U.S. Environmental Protection Agency
Office of Policy
1200 Pennsylvania Avenue NW, Mail Code 1803A
Washington, DC 20460
Re: Comments Regarding EPA’s Executive Order 13777, “Enforcing the Regulatory Reform Agenda,” Docket No. EPA-HQ-OA-2017-0190-0042, Comments from the National Center for Healthy Housing, David E. Jacobs, PhD, CIH, Chief Scientist
The National Center for Healthy Housing (NCHH) believes that elimination of funding for and so-called “reform” of EPA’s renovation, repair, and painting and abatement regulations under TSCA Title 4 will cause increased lead exposure to both children and workers, similar to the situation that prevailed before the regulations were in place. We urge EPA to enforce these regulations, not abandon them, weaken them, or render them toothless. The regulations are based on science. Industry groups, such as the Lead and Environmental Hazards Association, have asked EPA to create a level playing field so that renovation, repair, and painting (RRP) firms and abatement, inspection, and risk assessment firms are properly trained with the rules fully enforced. We also believe that EPA should update and strengthen its lead dust standards, pursuant to the advice of its own Science Advisory Board (NCHH’s Chief Scientist participated in the deliberations of the lead dust panel of the Science Advisory Board).
We offer these comments because we believe a return to a world without the protections offered by EPA’s lead poisoning prevention regulations and programs will allow dangerous and unnecessary methods of removing or disturbing lead paint that are widely known to cause harm. Indeed, these methods are already widely prohibited, but without the EPA regulations and enforcement, they will likely be used.
EPA specifically asked for the following information on whether EPA’s lead regulations:
(i) Eliminate jobs or inhibit job creation;
The evidence plainly shows that the EPA’s lead poisoning prevention regulations do not eliminate jobs or job creation. In fact, the evidence shows that the regulations help to create jobs for lead abatement and renovation, repair, and painting workers and firms. A partial listing of such firms is at
http://www.leadsafelist.com/renovators/. Furthermore, lists of abatement, risk assessment, and inspection personnel are available from each state or from EPA.
(ii) Are outdated, unnecessary, or ineffective;
The comments provided below demonstrate that abatement, inspection, risk assessment, and trained renovation, repair, and painting are all effective and necessary in reducing lead hazards. The EPA lead dust hazard standards are outdated and should be updated, as recommended by EPA’s own Science Advisory Board.
(iii) Impose costs that exceed benefits;
Benefits far exceed costs, as detailed below. There is no need to update the cost-benefit analyses for lead poisoning prevention regulations, because numerous cost-benefit studies have already been completed and show that the benefits far outweigh the costs. This assessment is not affected by the absence of lead test kits.
(iv) Create a serious inconsistency or otherwise interfere with regulatory reform initiatives and policies.
EPA regulations are consistent and do not interfere with other reform initiatives.
Background
Despite progress in recent years, blood lead levels remain a hundred times above background blood lead levels (Figure 1).1 According to the most recent peer reviewed publication, there are over 535,000 children with elevated blood lead levels (above 5 µg/dL, the CDC reference value) in the United States.2 Preventing childhood exposure to lead has a large return on investment; every dollar invested in lead hazard control results in health, educational, and other savings of between $17-221,3 a return slightly better than even vaccines. However, the Flint water crisis reminds us that investment in these interventions must not only be widespread but sustained, and that much more needs to be done to eliminate childhood lead poisoning. In the U.S., 37 million older homes contain lead paint, and 23 million of them have significant lead paint hazards.4 An estimated 3.6 million of these homes currently house young children (whose brains are still developing); children of color and children of low-income households are disproportionately impacted by lead exposures in these homes. In addition, an estimated 6.1 million homes have lead service lines for their drinking water.5
The most recent data from the CDC’s National Health and Nutrition Examination Survey showed that the average (i.e., geometric mean) blood lead levels among younger children, those belonging to poor families, and those enrolled in Medicaid were significantly higher compared with their older or more affluent counterparts. Furthermore, blood lead levels for non-Hispanic black children were significantly higher compared with either non-Hispanic white or Mexican-American children.6
Abatement is regulated by EPA and is effective in protecting children. Evidence for abatement effectiveness can be gleaned from several studies. The largest study is the Evaluation of the HUD Lead Hazard Control Grant program,7 a study covering over 3,000 housing units in 14 jurisdictions. Blood lead levels declined 37% two years after treatment. But because blood lead levels are affected by all sources of exposure, dust lead levels are likely to be a better metric of abatement effectiveness because they are less confounded by other sources of lead. Blood lead and dust lead are well correlated with each other in numerous studies.8, 9 Three years after intervention average (geometric mean) dust lead loadings on floors, windowsills, and window troughs declined by 78%, 89%, and 95%, respectively, compared to pre-intervention levels. These substantial declines were observed across all 14 jurisdictions in the study. The study also found that after controlling for other factors, full interior lead abatement was associated with the largest relative reductions in floor dust lead loadings over a year. But this can only work if there are trained certified abatement workers who know how to do the work properly.
Lead-safe renovation, repair, and painting, also regulated by EPA, is also effective in protecting children. For example, there are two principal studies of window replacement: One is a 12-year follow-up in four cities in the HUD Evaluation study, and the second is a recently completed study in Illinois. Both studies show large, sustained reduction in dust lead levels associated with window replacement. The most recent study10 shows that one year after window replacement, average (geometric mean) lead dust for interior floors, interior windowsills, and exterior window troughs declined by 44%, 88%, and 98%, respectively (P < .001).
Figure 1. “Natural” Background Blood Lead Levels from Flegal et al.
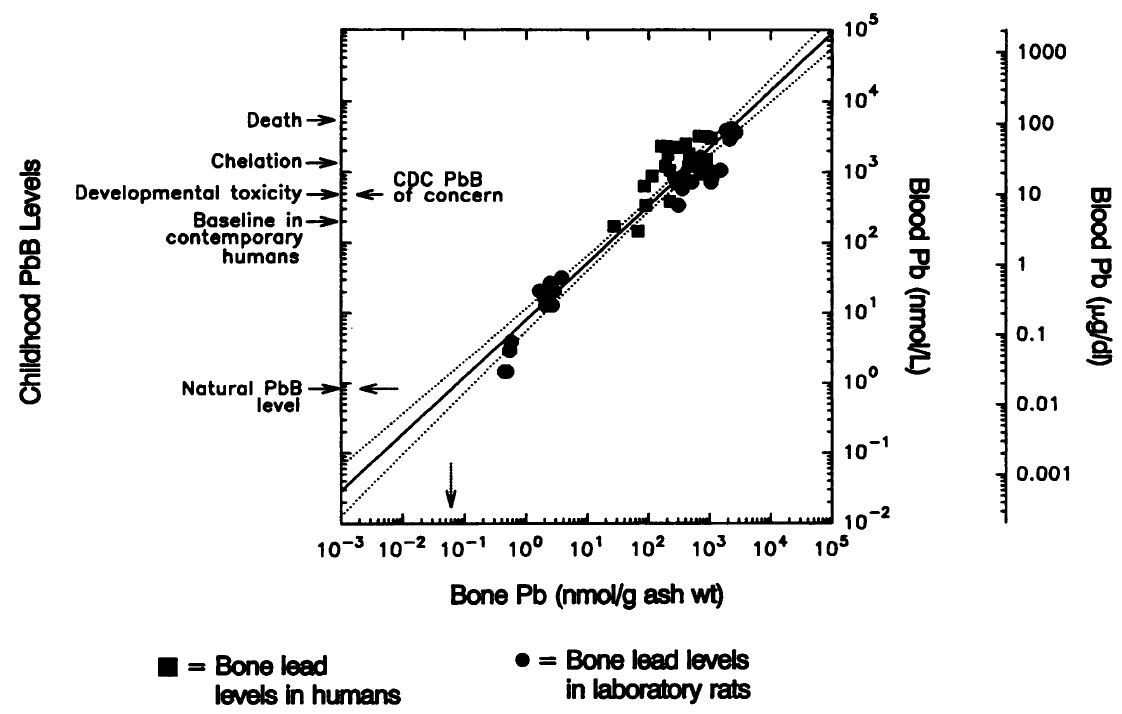
Note: The natural lead concentration in blood of humans (0.8 nmol/L or 0.016 µg/dL, dashed arrow on the ordinate) was derived from the reported concentrations of lead in pre-industrial human bone (dashed arrow on the abscissa) by graphical extrapolation of the relationship between paired bone-and blood- lead concentrations of humans (squares) and laboratory rats (circles). See Flegal and Smith for details.
The second study,11 which is also the nation’s longest-term follow-up study of lead-safe work practices, examined the relative difference in dust lead levels in homes in the HUD lead grant program that had none, some, and all windows replaced. Twelve years after intervention, homes with all replacement windows had 41% lower interior floor dust lead levels, compared to nonreplacement homes, and windowsill dust lead was 51% lower while controlling for covariates. Homes with only some windows replaced had interior floor and windowsill dust lead loadings that were 28% and 37% lower, respectively, compared to non-replacement homes. The net economic benefit of window replacement compared to window repair (nonreplacement) is $1,700–$2,000 per housing unit. Window replacement is a common hazard control practice that is regulated by EPA under its RRP regulation.
Importantly, both these studies showed large declines in dust lead levels, not only on windows as expected but also on floors, which children are likely to contact more frequently. These reductions occurred because lead-safe work practices were vigorously enforced.
In short, abatement and lead-safe renovation, repair, and painting, all of which are currently regulated by EPA, are effective and should not be weakened.
Specific Comments
The current prohibited practices (see Table 1) found throughout the vast fabric of state, local, and federal regulations regarding lead dust are predicated upon the decades of scientific research and human epidemiological studies that the federal government, including EPA, has funded for the last 30 years. The prohibited practices are based on the wisdom generated by those studies. The prohibitions are important because they are protective of human health in a scientifically demonstrable way.
There is little question that removing or disturbing lead paint without proper controls causes substantial contamination, posing serious risks to occupants, workers, and others, which is precisely why lead-safe work practices must be enforced, not weakened. At least eight studies support this contention.12, 13, 14, 15, 16, 17, 18, 19 For example, one study found that children with blood lead levels greater than or equal to 10 µg/dL were six times more likely to live in homes that had dust from painted surface preparation and lack of lead-safe work practices.20 Another study showed that the use of power sanding on the exterior of a house undergoing repainting resulted in soil lead levels in the child’s play area of over 130,000 ppm and interior floor dust lead levels of 27,600 micrograms per square foot (the respective EPA standards are 400 ppm and 40 micrograms per square foot). In this case study, the cleanup costs were nearly $200,000 for a single house21; these costs could have been entirely avoided if a safer method of paint removal were used instead.
In another case, which was detailed in the peer-reviewed and scientifically based HUD guidelines,22 the following is documented:
“Figure 4.1 A Case Report: Renovation and Lead Poisoning.
“The Marino case report (Marino, 1990) is an example of how uncontrolled renovation work can cause lead poisoning in both adults and children. The dwelling involved was a 2-story, 19th century Victorian farm house with 10 rooms. Most of the wooden floors, moldings, walls, ceilings, and door frames had been painted with lead-based paint. The renovation work included restoration of surfaces by removing the paint down to the bare surface on floors and woodwork and recoating with new varnish. Ceilings were repaired, and wallpaper and paint were removed from a number of walls. Two workers used rotary power sanders, hand sanders, scrapers, torches, heat guns, and chemical paint strippers. The family left the house during most of the renovation work, but returned after it was only partially completed. There was dust throughout the dwelling. After one of the family’s dogs started to have seizures, a veterinarian determined that the dog was lead poisoned. The mother and two children were subsequently tested. The children had blood lead levels of 104 micrograms per deciliter and 67 micrograms per deciliter, which is much higher than the blood lead reference value established by the Centers for Disease Control and Prevention (CDC) (5 micrograms per deciliter). The mother had a blood lead level of 56 micrograms per deciliter. All three were admitted to a local hospital where they were treated for severe lead poisoning. The mother was 8 weeks pregnant and opted for a therapeutic abortion. A babysitter who had two children of her own sometimes cared for all four children in the home. The babysitter’s two children were also tested and found to have blood lead levels of 80 micrograms per deciliter and 68 micrograms per deciliter. These two children were also hospitalized and treated for severe lead poisoning.”
To prevent these kinds of high exposure, EPA put significant lead-safe work practices and other control measures in place. These measures have been studied extensively and are effective. Among other preventive measures, they include work practices that minimize the creation of lead dust, containment, occupant protection, special cleaning methods, and quality control in the form of clearance testing and training and certification of workers.
EPA’s regulations include the following prohibitions:
Table 1. Prohibited Methods
(a) Open-flame burning or torching.
(b) Machine sanding or grinding without a high-efficiency particulate air (HEPA) local exhaust control.
(c) Abrasive blasting or sandblasting without HEPA local exhaust control.
(d) Heat guns operating above 1100 degrees Fahrenheit or charring the paint.
(e) Dry sanding or dry scraping, except dry scraping in conjunction with heat guns or within 1.0 foot (0.30 m.) of electrical outlets, or when treating defective paint spots totaling no more than 2 square feet (0.2 square meters) in any one interior room or space, or totaling no more than 20 square feet (2.0 square meters) on exterior surfaces.
(f) Paint stripping in a poorly ventilated space using a volatile stripper that is a hazardous substance in accordance with regulations of the Consumer Product Safety Commission at 16 CFR 1500.3, and/or a hazardous chemical in accordance with the Occupational Safety and Health Administration regulations at 29 CFR 1910.1200 or 1926.59, as applicable to the work.
The prohibition of dangerous methods of paint removal is a type of engineering control. Rather than attempting to control emissions after they have occurred, engineering controls are designed to prevent or minimize emissions from occurring in the first place and are frequently cited in other EPA, HUD, and OSHA regulations as being the best method.
EPA’s renovation, repair, and painting and abatement regulations should be enforced, not eliminated, as the President’s proposed budget does. The reasons are as follows:
1. The amount of lead dust that can be released from even a small area with a low concentration of lead-based paint undergoing torching, blasting, or power sanding is quite large.
To understand how easily leaded dust hazards can be created from jobs disturbing lead-based paint, consider the following example: Suppose renovation work is done on only one square foot of painted surface and all the lead paint inside that square foot is turned into dust (or fume) by sanding or some other work (such as torching). If the paint has one milligram per square centimeter of lead in it (the lowest level regulated by EPA) and if the dust is spread out over a 100-square-foot area (a 10-foot by 10-foot room), there will be about 9,300 micrograms per square foot of leaded dust present. This is much higher than the current EPA dust lead hazard standard for floors, which is 40 micrograms of lead dust per square foot. In short, suggestions that the de minimis definitions in the current rule should be revised are not founded on good science.
2. Prohibited work practices (if allowed under the EPA Administration’s attempt to eliminate regulations) pose substantial risks to current and future occupants, as well as workers and pedestrians and those in nearby properties.
So-called “traditional” lead-based paint removal methods that were employed between 1970 and about 1990 (before the implementation of EPA’s lead regulations) sometimes resulted in increases, not decreases in the blood lead level of children who lived in those houses, especially if baseline blood lead levels were low.23 A common practice in these early efforts involved the use of fuel-powered torches and power sanding to remove lead paint rapidly. In those years, the importance of controlling settled dust from lead paint was not fully understood. It is now clear that lead-contaminated settled dust is the principal exposure pathway for children in the U.S. today. Lead exposures to workers burning or power-sanding lead paint have been shown to be orders of magnitude larger than OSHA’s “permissible exposure limit,” ranging as high as 11,000 micrograms of lead per cubic meter.24 With airborne levels as high as this, it is likely that nearby properties will also become contaminated, posing risks to other innocent parties. These high exposures to workers, children, pedestrians, and nearby residents can all be avoided if such paint removal practices are prohibited and replaced by safer methods. The current EPA regulations help to prevent these large exposures.
3. There are safer methods of removing lead-based paint that are known, feasible, and effective.
One of the largest studies of lead paint hazard control in housing, covering nearly 3,000 housing units in 14 jurisdictions across the country, showed that modern methods of removing or disturbing lead paint, which included building component replacement, offsite and onsite paint stripping using chemicals, and wet scraping were effective and could be performed safely.25 The use of these methods did not produce large amounts of lead fume or settled lead dust, and the dust that was generated could be cleaned fairly easily. The EPA rules are based on studies such as this and should be retained.
Thank you for the opportunity to provide these comments. We believe the scientific evidence clearly shows that EPA’s lead poisoning prevention regulations, for abatement; for renovation, repair, and painting; and for disclosure and other related existing regulations should be enforced, not weakened. The evidence clearly shows that the regulations are feasible, economical, create jobs, and—most importantly—will protect the health of workers, children, pregnant women, those in nearby properties, and other at-risk populations.
Sincerely,
David E. Jacobs, PhD, CIH
Chief Scientist
National Center for Healthy Housing
National Safe and Healthy Housing Coalition
_______________
References
3 Gould, E. (2009, July). Childhood lead poisoning: Conservative estimates of the social and economic benefits of lead hazard control. Environmental Health Perspectives, 117(7), 1162-1167. Retrieved May 2, 2017, from https://ehp.niehs.nih.gov/0800408/
5 Cornwell, D. A., Brown, R. A., & Via, S. H. (2016, April). National survey of lead service line occurrence. Journal—American Water Works Association, 108(4), E182-E191. Retrieved May 2, 2017, from https://www.awwa.org/publications/journal-awwa/abstract/articleid/57880483.aspx
7 National Center for Healthy Housing & University of Cincinnati Department of Environmental Health. (2004, May 1). Evaluation of the HUD lead hazard control grant program: Final report. Columbia, MD: National Center for Healthy Housing. Retrieved May 2, 2017, from
http://www.hud.gov/offices/lead/library/misc/NatEval.pdf
8 Lanphear, B. P., Matte, T. D., Rogers, J., Clickner, R. P., Dietz, B., Bornschein, R. L., et al. (1998, October). The contribution of lead-contaminated house dust and residential soil to children's blood lead levels: A pooled analysis of 12 epidemiologic studies. Environmental Research, 79(1), 51-68. Retrieved May 2, 2017, from https://www.ncbi.nlm.nih.gov/pubmed/9756680
9 Lanphear, B. P., Emond, E., Jacobs, D. E., Weitzman, M., Tanner, M., Winter, N. L., Yakir, B., & Eberly, S. (1995, February). A side-by-side comparison of dust collection methods for sampling lead-contaminated house dust. Environmental Research, 68(2), 114-123. Retrieved May 2, 2017, from http://www.sciencedirect.com/science/article/pii/S0013935185710158
10 Jacobs, D. E., Tobin, M.,Targos, L., Clarkson, D., Dixon, S. L. Breysse, J., et al. (2016, September-October). Replacing windows reduces childhood lead exposure: Results from a state-funded program. Journal of Public Health Management & Practice, 22(5), 482-491. Retrieved May 2, 2017, from https://www.ncbi.nlm.nih.gov/pubmed/26910871
11 Dixon, S. L., Jacobs, D. E., Wilson, J. W., Akoto, J. Y., & Clark, C. S. (2012, February). Window replacement and residential lead paint hazard control 12 years later. Environmental Research, 113, 14-20. Retrieved May 2, 2017, from http://www.ncbi.nlm.nih.gov/pubmed/22325333
12 Rabinowitz, M., Leviton, A., Bellinger, D. (1985). Home refinishing, lead paint, and infant blood lead levels. American Journal of Public Health, 75(4), 403-404. Retrieved May 2, 2017, from https://www.ncbi.nlm.nih.gov/pubmed/3976969
14 Farfel, M. R., & Chisolm, J. J. Jr. (1990, October). Health and environmental outcomes of traditional and modified practices for abatement of residential lead paint. American Journal of Public Health, 80(10), 1240-1242, Retrieved May 2, 2017, from https://www.ncbi.nlm.nih.gov/pubmed/2136329
15 Amitai, Y., Graef, J. W., Brown, M. J., Gerstle, R. S., Kahn, N., Cochrane, P. E. (1987, July). Hazards of ‘deleading’ homes of children with lead poisoning. American Journal of Diseases of Children, 141(7), 758- 760. Retrieved May 2, 2017, from https://www.ncbi.nlm.nih.gov/pubmed/2438931
16 Swindell S. L., Charney, E., Brown, M. J., Delaney, J. (1994, September 1). Home abatement and blood lead changes in children with class III lead poisoning. Clinical Pediatrics, 33(9), 536-541. Retrieved May 2, 2017, from http://journals.sagepub.com/doi/abs/10.1177/000992289403300905?journalCode=cpja
18 Fischbein, A,, Anderson, K. E., Sassa, S., Lillis, R., Kon, S., Sarkozi, L., et al. (1981, April). Lead poisoning from “do-it-yourself” heat guns for removing lead paint: Report of two cases. Environmental Research, 24(2), 425-431. Retrieved May 2, 2017, from http://www.sciencedirect.com/science/article/pii/0013935181901705
19 Marino, P. E., Landrigan, P. J., Graef, J., Nussbaum, A., Bayan, G., Boch, K., et al. (1990, October). A case report of lead paint poisoning during renovation of a Victorian farmhouse. American Journal of Public Health, 80(10), 1183-1185. Retrieved May 2, 2017, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1404824/
20 Reisman, D. B., Matte, T. D., Gurnitz, K. L., Kaufmann, R. B., & Leighton, J. (2002, December). Is home renovation a risk factor for exposure to lead among children residing in New York City? Journal of Urban Health, 79(4), 502-511. Retrieved May 2, 2017, from https://www.ncbi.nlm.nih.gov/pubmed/12468670
21 Jacobs, D. E., Mielke, H., & Pavur, N. (2003, February). The high cost of improper removal of lead-based paint from housing: A case report. Environmental Health Perspectives, 111, 185-186. Retrieved May 2, 2017, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1241348/
23 Aschengrau, A., Beiser, A., Bellinger, D., Copenhafer, D., & Weitzman, M. (1987, October). Residential lead- based-paint hazard remediation and soil lead abatement: Their impact among children with mildly elevated blood lead levels. American Journal of Public Health, 87(10), 1698-1672. Retrieved May 2, 2017, from https://www.ncbi.nlm.nih.gov/pubmed/9357358
Also see NIOSH, HETA 99-0113-2853, HETA 93-0818-2646, HETA 96-0200-2799, HETA 98-0285-2989 NIOSH, HETA 99-0113-2853, HETA 93-0818-2646, HETA 96-0200-2799, HETA 98-0285-2989), which showed that these methods generate large amounts of lead in settled dust (HETA 98-0285-2989, 99-0113- 2853). NIOSH evaluations have found that technically feasible and effective alternatives to hazardous activities exist, including power sanding with HEPA exhaust control (NIOSH, HETA 99-0113-2853, HETA 93-0818-2646, HETA 96-0200-2799, HETA 98-0285-2989, HETA 92-095-2317).
25 National Center for Healthy Housing & University of Cincinnati Department of Environmental Health. (2004, May 1). Evaluation of the HUD lead hazard control grant program: Final report. Columbia, MD: National Center for Healthy Housing. Retrieved May 2, 2017, from http://www.hud.gov/offices/lead/library/misc/NatEval.pdf